Discover how the BLM gene affects diabetes risk, symptoms, and treatment. Learn about testing, management, and hope through new research and community support for BLM for Diabetes.
Understanding What BLM Is and How It Connects to Diabetes
Have you ever heard of Bloom Syndrome (BLM) and wondered how it’s linked to diabetes? Don’t worry — you’re not alone. Many people in the USA are starting to learn about this rare condition and how it affects the body in surprising ways. Let’s break it down together in the easiest way possible.
The BLM gene, also called RECQL3, acts like a repair worker for your body’s DNA. When this gene doesn’t work properly, it can cause something known as Bloom Syndrome — a rare genetic condition that can lead to a few health problems, including insulin resistance and diabetes mellitus (that’s the medical name for diabetes). Think of insulin as the key that lets sugar enter your body’s cells. When insulin doesn’t do its job right, sugar stays in your blood — and that’s where diabetes steps in.
People with Bloom Syndrome often have shorter height, sensitive skin, and a higher chance of developing type 2 diabetes at an early age. Researchers in the USA have also found that changes in the BLM gene make it harder for the body to control blood sugar. In simple words, when your DNA’s “fix-it crew” (the BLM gene) can’t keep up, your cells get confused, and your sugar levels start to rise.
Doctors recommend genetic testing for the BLM gene if someone shows signs of Bloom Syndrome or has a family history of it. Knowing early helps people manage their health better and lower the risks of insulin resistance and other related issues. This is especially important in families where autosomal recessive inheritance runs in the background — meaning both parents silently carry the same rare gene.
Even though Bloom Syndrome is rare, learning about it matters. It’s not just about understanding genes — it’s about giving real people the chance to live healthier, longer lives. With the help of genetic counseling, BLM gene testing, and better awareness, we can spot the signs early and treat diabetes before it becomes serious.
So, if you or someone you know struggles with unexplained insulin resistance, it might be worth checking the BLM gene connection. Because when it comes to health, the smallest piece of DNA can make the biggest difference.
How the BLM Gene Affects Insulin Resistance and Blood Sugar
Let’s dig a little deeper into how the BLM gene and diabetes are actually connected — but don’t worry, we’ll keep it simple.
Imagine your body as a busy city. Every cell is like a house that needs energy, and insulin is the delivery driver bringing that energy in the form of sugar. When everything runs smoothly, your cells stay powered up, and your blood sugar stays balanced.
But when there’s a problem with the BLM gene — the one responsible for fixing tiny mistakes in your DNA — it’s like the city’s repair crew going on break. Without proper repairs, the system becomes stressed, and over time, your body stops responding well to insulin. This is called insulin resistance, one of the biggest reasons people develop type 2 diabetes mellitus.
Scientists in the USA studying Bloom Syndrome (BLM) have found that when the BLM gene doesn’t work correctly, it can cause cell damage and confusion in how the body uses sugar for energy. This damage makes your cells less sensitive to insulin’s signal — kind of like when your phone keeps freezing and ignores your touch. The result? Sugar builds up in the blood instead of going into the cells, leading to high blood sugar and, eventually, diabetes.
People with Bloom Syndrome often show early signs of insulin resistance, sometimes even in childhood. The good news is that recognizing these signs early can make a huge difference. Through genetic testing for the BLM gene, doctors can confirm if someone’s insulin resistance is related to Bloom Syndrome, and then create a treatment plan to help manage it.
Understanding how BLM affects your blood sugar doesn’t just help doctors — it empowers families too. Parents who learn about autosomal recessive inheritance can take steps like genetic counseling to see if their children are at risk. It’s a smart move that gives you the upper hand in protecting your family’s health.
Remember, while Bloom Syndrome is rare, its link to diabetes teaches us something big: even the smallest gene in our DNA can play a huge role in how our body handles sugar. When you take care of your health, get tested early, and stay informed, you’re already one step ahead of insulin resistance.
Symptoms and Early Warning Signs of Bloom Syndrome and Diabetes
Spotting the signs early can make all the difference. When it comes to Bloom Syndrome (BLM) and diabetes, the body gives out tiny warning signals — you just need to know what to look for.
People with Bloom Syndrome often have a few unique traits that show up even from childhood. For example, they may be shorter than average, have sensitive skin that burns easily in the sun, and sometimes develop small red patches on the face called butterfly rashes. These are all common symptoms of BLM gene mutations. Since Bloom Syndrome is autosomal recessive, it means both parents must carry the same rare gene for a child to be affected — even if the parents don’t show symptoms themselves.
But that’s not all. One of the most important things to watch for is insulin resistance, which often leads to type 2 diabetes mellitus. Here’s what that can look like:
- Feeling tired all the time – Even after sleeping well, your body might feel drained because it can’t use sugar properly.
- Frequent thirst or hunger – High blood sugar can leave you constantly thirsty or craving snacks.
- Needing to pee often – When there’s too much sugar in the blood, your body tries to flush it out.
- Blurry vision – Unbalanced sugar levels can make your eyesight go fuzzy.
- Unexplained weight changes – Some people lose weight quickly, while others gain it — both can be early signs of diabetes.
Doctors in the USA often recommend genetic testing for the BLM gene if a patient has these symptoms along with a family history of Bloom Syndrome or early-onset diabetes. Early diagnosis is key — it allows doctors to monitor for other related issues such as immune problems or increased cancer risk, both of which are more common in people with Bloom Syndrome.
If you or someone in your family shows these warning signs, don’t ignore them. Talking to a doctor or genetic counselor can help you understand if the BLM gene might be involved. With early testing, you can manage insulin resistance, lower the risk of serious diabetes complications, and live a healthier, happier life.
Remember — listening to your body’s small signals today can protect your health tomorrow.
Diagnosis and Genetic Testing for the BLM Gene in the USA
Finding answers starts with the right tests. When doctors suspect Bloom Syndrome (BLM) or an early link to diabetes, the first step is to look closely at the BLM gene — the tiny piece of DNA responsible for it all.
In simple words, the BLM gene acts like a bodyguard for your DNA, fixing any damage that happens during cell growth. But when there’s a BLM gene mutation, this repair system breaks down, leading to conditions like Bloom Syndrome and even insulin resistance that can cause type 2 diabetes mellitus.
To confirm this, doctors recommend genetic testing for the BLM gene. It’s a painless process that usually starts with a small blood sample or a cheek swab. The sample is then sent to a lab, where scientists look for changes in the BLM (RECQL3) gene. If the test finds two abnormal copies of this gene, it confirms Bloom Syndrome — because the condition follows an autosomal recessive inheritance pattern.
In the USA, several certified labs and hospitals offer BLM gene testing. These include well-known centers like Mayo Clinic, Quest Diagnostics, and Invitae, which provide accurate results and follow-up genetic counseling. Some people also get tested through rare disease programs or university medical centers that specialize in genetic disorders.
After testing, doctors often discuss next steps with a genetic counselor. This is where families learn what the results mean, how Bloom Syndrome could affect health, and how to manage related risks — like diabetes or cancer susceptibility. Early detection allows doctors to monitor blood sugar levels, manage insulin resistance, and design treatment plans tailored for each person’s needs.
Getting tested doesn’t just answer questions; it provides peace of mind. Even if the results come back negative, you’ll know where you stand. And if they show a BLM gene mutation, you’ll have a clear path to follow — from managing diabetes to protecting your overall health.
So, if Bloom Syndrome or unexplained high blood sugar runs in your family, consider genetic testing for the BLM gene. It’s one of the smartest steps you can take toward early diagnosis and a healthier future.
Managing Diabetes When You Have Bloom Syndrome (BLM)
Living with both Bloom Syndrome (BLM) and diabetes might sound challenging — but it’s absolutely manageable with the right care and mindset. 💛 While science is still uncovering all the details about how the BLM gene affects insulin resistance, one thing is clear: a smart, consistent routine can help you stay strong and healthy every single day.

1. Balance Your Diet
Food is your body’s best medicine. People with BLM and diabetes should focus on whole grains, lean proteins, and fresh vegetables. Avoid sugary snacks and processed foods — they spike your blood sugar quickly.
Try to include fiber-rich options like brown rice, oats, and beans, which help stabilize glucose levels. Remember, moderation is the key. Even healthy foods can raise blood sugar if eaten in large amounts.
2. Stay Physically Active
Exercise doesn’t just keep your body fit — it improves insulin sensitivity, helping your cells use sugar more effectively. Aim for at least 30 minutes of movement daily, whether that’s walking, cycling, or yoga.
People with Bloom Syndrome should choose low-impact exercises, since the body can be more sensitive to physical stress. Consistency matters more than intensity.
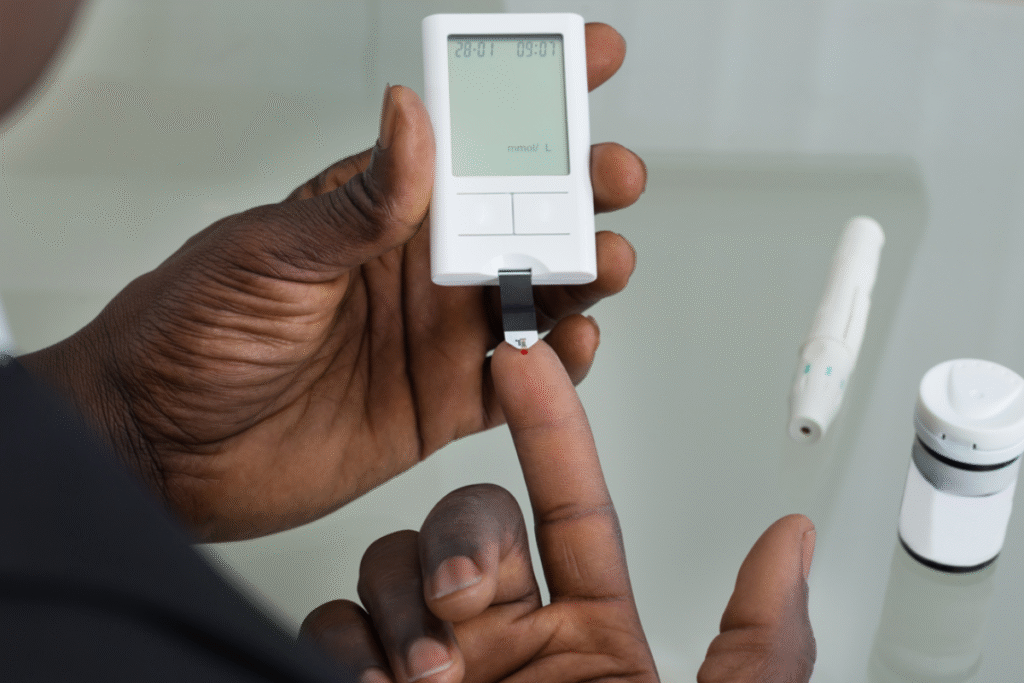
3. Regular Blood Sugar Monitoring
Keeping an eye on your blood sugar levels helps you catch changes early. Many people use home glucose monitors or continuous glucose sensors (CGMs) for better control.
If you have BLM gene mutations, your doctor may recommend more frequent monitoring, as your metabolism may react differently to insulin or medications.
4. Medication and Doctor Visits
Always follow your diabetes treatment plan closely. Some people may need oral diabetes medications or insulin injections to manage their sugar levels effectively. Regular checkups with your endocrinologist and genetic counselor are important to track progress and adjust treatment as needed.
5. Emotional and Mental Health
Managing a lifelong condition like BLM with diabetes can sometimes feel overwhelming — and that’s okay. Talk to family, join support groups, or connect with others online who share your experience. Emotional health is just as vital as physical care.
6. Preventive Care
Routine screenings are your best defense. People with Bloom Syndrome are more prone to immune problems and certain cancers, so regular health checkups are non-negotiable. Catching any change early makes treatment easier and more effective.
Living with BLM for diabetes is not about perfection — it’s about progress. Every smart food choice, every walk, and every doctor visit adds up to a stronger, healthier you. 🌿 With the right support and awareness, you can live fully and confidently, one day at a time.
New Research, Genetic Therapies, and Future Hope for BLM and Diabetes
Science never stops searching for answers — and that’s amazing news for people living with Bloom Syndrome (BLM) and diabetes. Researchers around the world are making exciting discoveries about how the BLM gene affects DNA repair, insulin resistance, and overall metabolism. Each study brings new hope for better treatments and, one day, maybe even a cure. 🌈
1. Genetic Therapy and DNA Repair Research
One of the most promising fields is gene therapy — a technique where scientists try to fix or replace the faulty BLM gene that causes Bloom Syndrome. In early lab studies, researchers have found ways to repair damaged DNA using advanced tools like CRISPR-Cas9. Although it’s still in experimental stages, this method could one day help correct BLM gene mutations directly, reducing the risk of diabetes and other complications.
2. Diabetes Management Innovations
At the same time, new diabetes treatments are emerging that may benefit people with BLM gene mutations. For example, GLP-1 receptor agonists — a new class of diabetes medications — help control blood sugar while also improving heart health and supporting weight management. Researchers in the USA are also testing artificial pancreas systems, which automatically adjust insulin delivery based on real-time glucose levels.
3. Precision Medicine
The future of healthcare is personal. With precision medicine, doctors can design customized treatment plans based on your genetic makeup — including whether or not you carry BLM gene mutations. This personalized approach means more effective diabetes management, fewer side effects, and better long-term results.
4. Lifestyle and Preventive Research
Recent studies also highlight how diet, sleep, and stress influence both Bloom Syndrome and diabetes. A balanced lifestyle rich in antioxidants, regular exercise, and proper sleep can strengthen DNA repair and improve insulin sensitivity. These findings remind us that even small, daily choices play a big role in long-term health.
5. Hope for the Future
Every discovery — big or small — adds to the growing hope for those affected by BLM for diabetes. Scientists are now connecting dots between genetic disorders and metabolic diseases, unlocking knowledge that could one day lead to prevention or reversal. And with continued funding, collaboration, and awareness, the future looks brighter than ever. ✨
Medical science has come a long way, but compassion and awareness are just as powerful. By staying informed and proactive, people with Bloom Syndrome and diabetes can look forward to longer, healthier, and happier lives. 💖
Living with BLM and Diabetes — Support, Awareness, and Community
Living with Bloom Syndrome (BLM) and diabetes isn’t just about managing medical tests and treatments — it’s about courage, hope, and connection. 💕 Every person facing BLM for diabetes has a story worth telling, and those stories are helping create a more understanding and supportive world.
1. Finding Strength in Community
You’re not alone on this journey. Across the USA, there are several support groups and nonprofit organizations dedicated to helping families affected by Bloom Syndrome and genetic diabetes. Online platforms such as RareConnect, Genetic Alliance, and Diabetes.org allow patients and caregivers to share advice, experiences, and encouragement.
Even local hospitals and universities often have genetic counseling centers where families can learn more about the BLM gene, insulin resistance, and blood sugar management options.
2. Raising Awareness
Awareness changes everything. Many people have never heard of Bloom Syndrome — and that’s why your voice matters. Sharing reliable information on social media, participating in rare disease events, or joining diabetes awareness walks can spread knowledge and inspire others. Every small effort helps bring genetic disorders like BLM Syndrome out of the shadows and into the public eye.
3. Emotional Wellbeing
It’s okay to feel overwhelmed sometimes — managing BLM and diabetes can be emotionally draining. That’s why mental health support is so important. Talking with a therapist, joining a support group, or simply opening up to friends and family can make a big difference. Remember: asking for help isn’t a weakness, it’s a sign of strength. 💪
4. Celebrating Small Wins
Health is a journey, not a race. Every balanced meal, every blood sugar check, and every doctor visit is a victory worth celebrating. The path to managing BLM with diabetes may not always be smooth, but every step forward brings new hope.
5. The Power of Knowledge
Knowledge empowers you to take control of your health. Understanding how the BLM gene mutation affects your body helps you make smarter choices — from diet to exercise to preventive care. And with new research and gene therapy advancing every year, the outlook for people living with Bloom Syndrome and diabetes continues to improve. 🌿
Living with BLM for diabetes is about more than a diagnosis — it’s about resilience, learning, and living fully. By embracing awareness, seeking support, and staying positive, you can turn challenges into strength and hope into healing. 💖
You are not defined by your condition — you’re defined by your courage.