Learn about diabetic neuropathy ICD 10 codes, meanings, and examples. Understand how ICD-10-CM helps with diagnosis, billing, and treatment in the U.S.
What Is Diabetic Neuropathy and Why the ICD-10 Code Matters

If you’ve ever heard a doctor mention diabetic neuropathy ICD 10, you might have wondered what that even means. Don’t worry — it’s not as complicated as it sounds. Let’s break it down together.
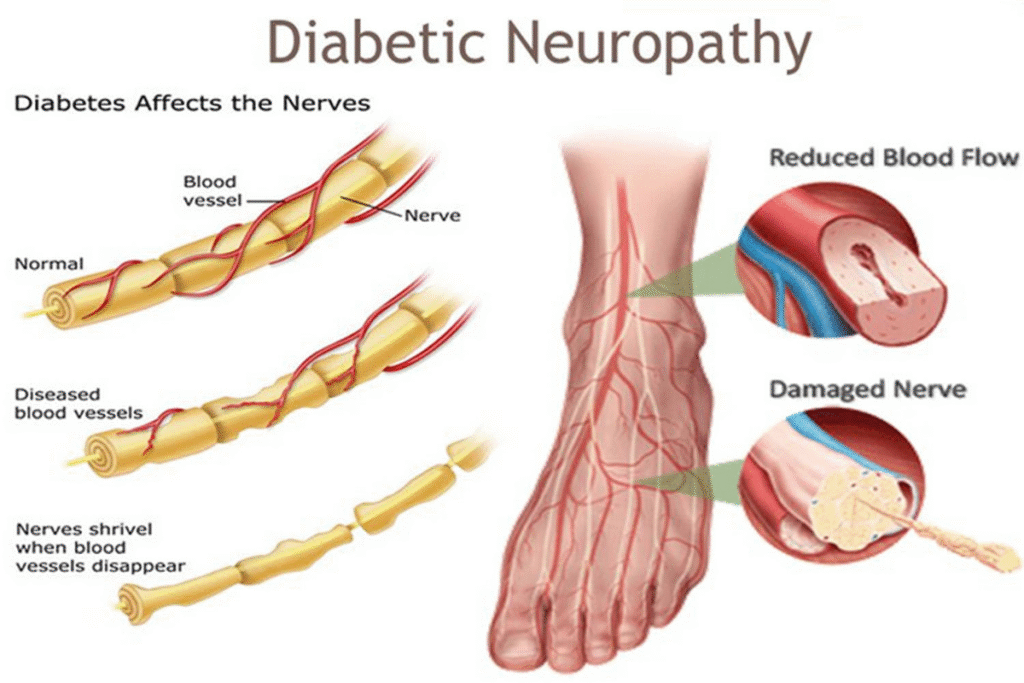
Diabetic neuropathy is a fancy term for nerve damage that happens when someone has diabetes for a long time. Think of your nerves like tiny electrical wires running through your body. When blood sugar levels stay high for too long, those “wires” can get damaged. This can cause tingling, numbness, or even pain in your hands and feet.
Now, here’s where the ICD-10 code for diabetic neuropathy comes in. In the medical world, every condition gets its own unique number — sort of like a barcode for diseases. These codes help doctors, hospitals, and insurance companies talk in the same “language.” So when a doctor writes E11.42, it tells everyone that the patient has type 2 diabetes with polyneuropathy. Cool, right? It’s a neat way to stay organized!
There are different codes for different types of diabetic neuropathy, such as:
- E11.40 – diabetic neuropathy, unspecified
- E11.41 – diabetic mononeuropathy
- E11.43 – diabetic autonomic neuropathy
- E11.44 – diabetic amyotrophy
- E11.49 – other diabetic neurological complications
Doctors use these ICD-10-CM diabetic neuropathy codes to record exactly what kind of nerve damage someone has. This matters a lot because using the wrong code can lead to billing errors or confusion about a patient’s health condition.
Here’s the fun part: the ICD-10 system isn’t just for type 2 diabetes. There are also special codes for type 1, such as E10.42, and for other forms like E13.42. So whether it’s diabetic polyneuropathy ICD-10 or diabetic autonomic neuropathy ICD-10, each number tells a clear story about what’s happening inside the body.
In short, ICD-10 coding for diabetic neuropathy is like a secret code that keeps hospitals, doctors, and patients all on the same page. It helps make sure everyone gets the right care, the right billing, and the right medical record — all thanks to a few smart numbers and letters.
Understanding the ICD-10-CM Diabetes Code Structure
Before diving deeper into diabetic neuropathy ICD 10, it helps to understand how the ICD-10-CM diabetes codes actually work. Imagine the ICD-10 system as a huge library — every disease, symptom, and medical condition has its own “book number” so doctors can find it quickly.
In the United States, these codes are part of a system called the ICD-10-CM (International Classification of Diseases, Clinical Modification). It’s used by doctors, hospitals, and insurance companies to track diagnoses and make sure everyone’s speaking the same medical language.
Each ICD-10 diabetes code starts with a letter (like E) followed by numbers. The letter shows the general category of the disease — in this case, E stands for “Endocrine, nutritional, and metabolic diseases.” The numbers that come after it tell us more details, such as the type of diabetes and what complications are involved.
For example:
- E11.42 = Type 2 diabetes mellitus with diabetic polyneuropathy
- E10.42 = Type 1 diabetes mellitus with diabetic polyneuropathy
- E13.42 = Other specified diabetes mellitus with diabetic polyneuropathy
See how the first two digits (E10, E11, E13) show the type of diabetes, while the numbers after the dot (like .42) show the specific complication — in this case, neuropathy.
Doctors and medical coders use these ICD-10 codes for diabetic neuropathy to record exactly what type of nerve damage is linked to diabetes. This level of detail helps in many ways:
- Accurate diagnosis – Doctors can identify the exact complication.
- Insurance billing – Claims get processed faster and with fewer errors.
- Patient care – It ensures each patient gets the right treatment.
It’s worth noting that before ICD-10, the world used ICD-9 codes, which were much simpler but less detailed. The upgrade to ICD-10 made medical coding far more precise. For example, instead of one general code for diabetic complications, ICD-10 offers several — like E11.40 for unspecified neuropathy and E11.43 for autonomic neuropathy.
In short, ICD-10 coding for diabetic neuropathy is like a GPS for healthcare. It guides professionals to the exact diagnosis, ensuring everything from hospital records to insurance claims stays clear and accurate.
Types of Diabetic Neuropathy and Their ICD-10 Codes
Now that you know what diabetic neuropathy ICD 10 means, let’s explore the different types of diabetic neuropathy and their specific ICD-10 codes. Each type affects the nerves in a unique way — and yes, each has its own special code in the medical world!
Think of it like different “versions” of the same condition. The core problem is nerve damage from diabetes, but where and how it affects the body can vary.
Here’s a simple breakdown 👇
1. Diabetic Polyneuropathy (ICD-10: E11.42)
This is the most common type. Diabetic polyneuropathy ICD 10 refers to nerve damage that affects many nerves at once, usually in the feet and hands. It can cause tingling, numbness, or burning pain — often worse at night. Doctors use E11.42 for type 2 diabetes with polyneuropathy, and E10.42 if it’s type 1 diabetes.
2. Diabetic Mononeuropathy (ICD-10: E11.41)
Here, “mono” means one — so diabetic mononeuropathy ICD 10 describes damage to a single nerve. This could be a nerve in your leg, arm, or even face. It’s less common but can cause sudden weakness or pain in one specific area.
3. Diabetic Autonomic Neuropathy (ICD-10: E11.43)
Your body does many things automatically — like controlling your heartbeat, digestion, and blood pressure. When those nerves are affected, it’s called diabetic autonomic neuropathy ICD 10, and the code E11.43 is used. Symptoms can include dizziness, stomach problems, or bladder issues.
4. Diabetic Amyotrophy (ICD-10: E11.44)
This one’s a bit rarer. Diabetic amyotrophy ICD 10 points to nerve damage that causes muscle weakness, especially in the thighs or hips. People might feel pain, then notice their legs getting weaker over time. The code for this is E11.44, and it’s often linked with sudden weight loss.
5. Other Diabetic Neurological Complications (ICD-10: E11.49)
If a patient’s symptoms don’t fit neatly into any of the categories above, doctors use the code E11.49 for other diabetic neurological complications. This ensures nothing gets left out of the diagnosis process.
6. Unspecified Diabetic Neuropathy (ICD-10: E11.40)
Sometimes doctors know there’s nerve damage related to diabetes but don’t yet know the exact type. In those cases, E11.40 — diabetic neuropathy unspecified ICD 10 — is used as a temporary placeholder until further testing is done.
Each of these ICD-10-CM diabetic neuropathy codes helps healthcare providers be specific and accurate. The more precise the coding, the better the patient care, insurance processing, and treatment outcomes.
In simple words, these codes act like medical “labels” — they tell the exact story of what’s happening inside your nerves. So, next time you see a code like E11.42 on your medical record, you’ll know it’s not just a random number. It’s a snapshot of your health — short, clear, and powerful.
Common Symptoms and Early Warning Signs of Diabetic Neuropathy
Knowing the symptoms of diabetic neuropathy can make a huge difference — especially if you catch them early. The sooner you notice something feels “off,” the sooner you can talk to your doctor and get the right care.
Diabetic neuropathy ICD 10 may look like just a code in your health record, but behind that number are real signs your body sends to warn you something’s wrong.
Here’s what to watch for 👇
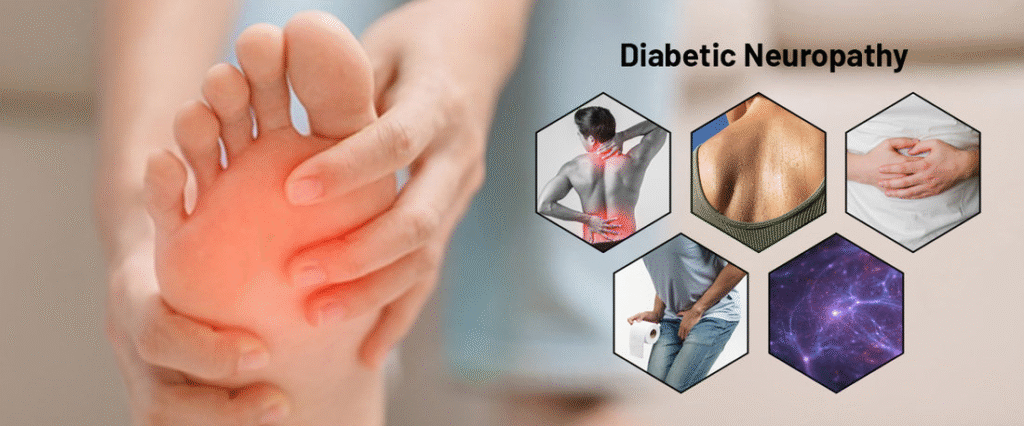
1. Tingling or Numbness in Hands and Feet
This is one of the first and most common symptoms of diabetic polyneuropathy ICD 10. It feels like tiny pins and needles, or sometimes a loss of feeling altogether. You might not notice small cuts or burns because the nerves in your hands and feet can’t send signals properly.
2. Burning or Sharp Pain
Some people feel a burning, stabbing, or shooting pain, especially at night. This pain can make it hard to sleep and is often linked with diabetic peripheral neuropathy ICD 10.
3. Weakness or Muscle Loss
If you have trouble standing, walking, or lifting things, it could be a sign of diabetic amyotrophy ICD 10 — a rare type that affects muscles in the thighs or hips. Over time, your muscles may feel weaker or smaller.
4. Dizziness or Fainting
Feeling dizzy when standing up can be a clue to diabetic autonomic neuropathy ICD 10. That’s because your blood pressure and heart rate are controlled by nerves that may not be working properly.
5. Digestive or Bladder Problems
Nerves also help control your stomach and bladder. If you notice bloating, constipation, or trouble urinating, these could be early signs of diabetic autonomic neuropathy.
6. Loss of Balance or Coordination
Because diabetic neuropathy affects how your nerves send messages to your brain, you might find it harder to balance or walk straight. This symptom can appear in people with long-term diabetes or poor blood sugar control.
7. Sexual Dysfunction
For both men and women, diabetic autonomic neuropathy ICD 10 may also cause problems like erectile dysfunction or reduced sensation, due to nerve damage affecting blood flow and organ control.
These symptoms often start mild but can get worse over time if blood sugar stays high. What’s tricky is that some people don’t feel pain at all — their nerves are so damaged that signals simply stop reaching the brain. That’s why regular checkups and accurate ICD-10 coding for diabetic neuropathy are so important.
If you notice any of these early warning signs, don’t ignore them. Talk to your doctor right away. With proper diagnosis, using codes like E11.42 or E11.43, you can get on a treatment plan that helps prevent further damage and keeps your nerves healthy.
Remember: catching diabetic neuropathy early can save you from serious complications later — and that’s something worth paying attention to.
Diagnosis and ICD-10 Documentation Process for Diabetic Neuropathy
Getting the right diagnosis for diabetic neuropathy is more than just noticing symptoms — it’s about using the right medical tests and assigning the correct ICD-10 code so everything is properly documented. Accurate ICD-10 coding for diabetic neuropathy ensures doctors, hospitals, and insurance companies are all on the same page about your health condition.
1. How Doctors Diagnose Diabetic Neuropathy
Doctors start by checking your medical history, blood sugar control, and any symptoms like tingling, numbness, or pain. They might perform a physical exam to test reflexes, muscle strength, and how well you feel sensations in your hands or feet.
Some common tests include:
- Nerve conduction studies – to see how well your nerves send signals.
- Electromyography (EMG) – to test muscle activity.
- Monofilament test – a simple test to check for sensation loss in your feet.
These tests help identify what type of neuropathy you have — whether it’s diabetic polyneuropathy ICD 10 (E11.42), diabetic autonomic neuropathy ICD 10 (E11.43), or diabetic amyotrophy ICD 10 (E11.44).
2. Importance of Accurate ICD-10 Coding
Once your doctor determines the type of neuropathy, they record it using the most specific ICD-10-CM diabetic neuropathy code possible. This is important because even a small mistake in documentation can cause issues with treatment plans or insurance billing.
Here’s a quick recap of the most used codes:
- E11.40 – Diabetic neuropathy, unspecified
- E11.41 – Diabetic mononeuropathy
- E11.42 – Diabetic polyneuropathy
- E11.43 – Diabetic autonomic neuropathy
- E11.44 – Diabetic amyotrophy
- E11.49 – Other diabetic neurological complications
For type 1 diabetes, the same format applies — just replace E11 with E10, for example, E10.42 for diabetic polyneuropathy due to type 1 diabetes.
3. ICD-10 Documentation Process
The documentation process starts with the physician noting symptoms, clinical findings, and test results in the patient’s record. Then, a medical coder assigns the most accurate ICD-10 code for diabetic neuropathy based on those notes.
This code not only tells insurers what condition the patient has but also ensures they get the correct coverage and care. It’s also essential for medical research and public health statistics — helping experts understand how common diabetic nerve damage really is.
4. The Role of E.E.A.T in Medical Documentation
In healthcare writing and documentation, E-E-A-T (Experience, Expertise, Authoritativeness, and Trustworthiness) plays a key role. Patients trust their medical providers when information is accurate, clear, and well-documented. That’s why using correct ICD-10-CM codes for diabetic neuropathy shows professionalism and care in every step of the process.
Accurate diagnosis and documentation might sound like paperwork, but they’re the backbone of proper treatment. A well-chosen diabetic neuropathy ICD 10 code can mean the difference between getting the right care and missing out on crucial treatment.
So, when your doctor notes a code like E11.42, know that it’s not just a number — it’s a signal that your health is being carefully recorded and managed.
Treatment and Management of Diabetic Neuropathy (Using the ICD-10 Framework)
Once a doctor confirms your diagnosis with the right diabetic neuropathy ICD 10 code, the next step is creating a solid treatment plan. The good news? While diabetic neuropathy can’t always be reversed, it can be managed — and even slowed down — with the right care and lifestyle habits.
Let’s break down how it’s treated and how ICD-10 coding helps guide that process.
1. Why ICD-10 Codes Matter in Treatment
Each ICD-10-CM diabetic neuropathy code gives doctors precise details about what type of nerve damage you have. For example, E11.42 (diabetic polyneuropathy ICD 10) tells the care team that multiple nerves are affected, while E11.43 (diabetic autonomic neuropathy ICD 10) signals that internal organ nerves are involved.
This accuracy helps healthcare providers:
- Design personalized treatment plans based on the type and severity of nerve damage.
- Monitor progress using consistent medical records.
- Ensure proper insurance coverage for medications and therapies.
Simply put — coding isn’t just paperwork. It’s a roadmap for care.
2. Medical Treatments for Diabetic Neuropathy
Treatment usually focuses on three goals:
- Controlling blood sugar levels
- Easing nerve pain
- Preventing further nerve damage
Here’s how doctors approach it:
- Blood sugar control: Keeping glucose levels stable is the #1 step to protect your nerves.
- Pain relief: Medications like pregabalin or duloxetine are often prescribed for diabetic peripheral neuropathy ICD 10 cases.
- Nerve repair support: Vitamin B12 supplements and certain therapies may help nerves heal.
- Foot care: Since many patients develop diabetic polyneuropathy, daily foot checks are vital to avoid infections or ulcers.
3. Lifestyle and Home Management Tips
Even small daily changes can make a big impact. Here’s what experts recommend:
- Eat balanced meals with fiber, lean protein, and fewer sugary foods.
- Stay active — walking or swimming improves blood flow to your nerves.
- Avoid smoking and limit alcohol, as both worsen nerve damage.
- Check your feet daily and wear comfortable shoes to prevent injuries.
For those coded with E11.42 or E11.43, following these steps consistently can help reduce pain, improve mobility, and slow disease progression.
4. Complementary Therapies
In addition to medication, some patients find relief through:
- Physical therapy – to improve strength and balance.
- Acupuncture – can ease nerve pain in some cases.
- Massage or relaxation techniques – to lower stress and muscle tension.
While these may not replace medical treatments, they can enhance your overall well-being when used alongside your main care plan.
5. Continuous Monitoring and Documentation
Every follow-up visit allows your healthcare provider to update your medical record using the appropriate ICD-10 code for diabetic neuropathy. This helps track progress, identify new symptoms, and make adjustments to your treatment.
For example, if a patient moves from mild symptoms (E11.40) to specific polyneuropathy (E11.42), updating the code keeps everything accurate and transparent for insurance and future care.
In short, managing diabetic neuropathy is about teamwork — between you, your doctor, and the data in your medical record. Each ICD-10 diabetic neuropathy code plays a vital role in making sure you get the right care at the right time.
And remember: while numbers like E11.42 may seem cold or clinical, they represent something powerful — your path toward healing, understanding, and better health.
Prevention Tips and How ICD-10 Helps Track Diabetic Complications
The best way to deal with diabetic neuropathy is to prevent it before it starts. While the diabetic neuropathy ICD 10 code helps doctors record and manage the condition, prevention begins with your daily habits and consistent health checkups.
You don’t need to be a doctor to protect your nerves — just a few smart steps can go a long way toward keeping them healthy.
1. Keep Blood Sugar Levels in Check
This is your number one defense! Consistently high blood sugar damages nerves over time. Monitoring your glucose, following your treatment plan, and eating balanced meals can stop diabetic neuropathy before it takes hold.
Doctors often use ICD-10 coding for diabetic neuropathy to track complications caused by poor sugar control, such as E11.42 (diabetic polyneuropathy) or E11.43 (autonomic neuropathy). Keeping those numbers out of your medical chart should be the goal!
2. Get Regular Health Screenings
Early detection can change everything. Doctors recommend regular nerve checks, especially for your feet and legs, since that’s where most symptoms begin.
Each exam helps your doctor update or rule out conditions in your record using ICD-10-CM diabetic neuropathy codes. For example, if early signs of nerve damage appear, they may note E11.40 (diabetic neuropathy, unspecified) for monitoring.
3. Practice Good Foot Care
This might sound simple, but it’s powerful. Wash your feet daily, dry them well, trim nails carefully, and check for blisters or cuts. People with diabetic peripheral neuropathy ICD 10 often don’t feel small wounds — and those can turn serious quickly.
Wearing soft, cushioned shoes and avoiding barefoot walking can save you from infections or ulcers later on.
4. Stay Active and Eat Smart
Exercise boosts blood circulation and helps nerves stay healthy. Even a 20-minute walk after meals can make a big difference. Pair that with a diabetes-friendly diet — less sugar, more fiber, lean proteins, and healthy fats — and your body will thank you.
Remember: prevention isn’t about perfection. It’s about consistency.
5. Quit Smoking and Limit Alcohol
Both smoking and alcohol restrict blood flow, making it harder for your nerves to heal. Quitting now not only lowers your risk of diabetic neuropathy, but also improves your heart, eyes, and kidney health — all of which can be affected by diabetes.
6. How ICD-10 Helps in Long-Term Tracking
The ICD-10 system isn’t just about medical billing — it’s a powerful tool for tracking your overall diabetes journey. Doctors use it to see patterns over time:
- Has your condition improved or worsened?
- Are there new symptoms that point to another complication?
- Which treatments are working best for your ICD-10 diabetic neuropathy code type?
This data helps not only you but also healthcare researchers who study how to prevent diabetic neurological complications on a larger scale.
7. Work Closely with Your Care Team
The best prevention happens when you and your care team work together. Whether your chart shows E11.42, E11.43, or any other ICD-10-CM code, your doctor can use it to guide treatment, track progress, and adjust your plan as needed.
In short, diabetic neuropathy doesn’t happen overnight — and with consistent care, it doesn’t have to happen at all. The ICD-10 coding system gives doctors the tools to catch nerve problems early, while you have the power to stop them from getting worse.
So, keep your sugar steady, your feet happy, and your health records clean — because prevention is the best code your body can live by!
Conclusion and FAQs
Final Thoughts
Understanding diabetic neuropathy ICD 10 isn’t just about memorizing a medical code — it’s about understanding your health in a deeper way. Those small combinations of letters and numbers, like E11.42 or E11.43, tell an important story about what’s happening inside your body.
Each ICD-10-CM diabetic neuropathy code gives doctors the clarity they need to diagnose, treat, and track your condition. But your own awareness plays the biggest role of all. By recognizing early symptoms, managing blood sugar, and staying consistent with medical care, you can take real control over your health.
Here’s the truth: diabetic neuropathy doesn’t have to define your life. With the right knowledge, early detection, and a solid prevention plan, you can live well and stay ahead of complications.
So next time you see your doctor or review your report, remember — those ICD-10 diabetic neuropathy codes are more than paperwork. They’re powerful tools helping you get the care, coverage, and attention you deserve.
Stay informed, stay proactive, and keep your nerves — and numbers — in balance. 💙
Frequently Asked Questions (FAQs)
1. What is the ICD-10 code for diabetic neuropathy?
The general ICD-10 code for diabetic neuropathy is E11.40 (diabetic neuropathy, unspecified). However, there are more specific codes like E11.42 for diabetic polyneuropathy and E11.43 for diabetic autonomic neuropathy.
2. What does ICD-10-CM mean?
ICD-10-CM stands for International Classification of Diseases, 10th Revision, Clinical Modification. It’s the system used in the United States to classify and code all health conditions for accurate medical records, billing, and research.
3. What is the ICD-10 code for diabetic polyneuropathy?
The ICD-10 code for diabetic polyneuropathy is E11.42 (for type 2 diabetes) and E10.42 (for type 1 diabetes). These codes specify nerve damage affecting multiple nerves, often seen in the hands and feet.
4. Can diabetic neuropathy be reversed?
Unfortunately, diabetic neuropathy usually can’t be fully reversed, but its symptoms can be managed and progression slowed. Early treatment, proper blood sugar control, and healthy habits can prevent severe nerve damage.
5. Why are ICD-10 codes important for diabetic neuropathy?
ICD-10 diabetic neuropathy codes ensure that doctors and insurance companies understand exactly what kind of nerve damage a patient has. This accuracy improves treatment plans, billing, and patient outcomes.
6. What are the most common diabetic neuropathy ICD-10 codes used in the U.S.?
Some of the most common include:
- E11.40 – Diabetic neuropathy, unspecified
- E11.41 – Diabetic mononeuropathy
- E11.42 – Diabetic polyneuropathy
- E11.43 – Diabetic autonomic neuropathy
- E11.44 – Diabetic amyotrophy
- E11.49 – Other diabetic neurological complications
7. How does ICD-10 help prevent diabetic complications?
By keeping medical records precise, ICD-10-CM coding for diabetic neuropathy helps doctors monitor changes, spot early warning signs, and prevent severe complications through timely care and follow-up.
8. What’s the difference between diabetic neuropathy and peripheral neuropathy?
Diabetic neuropathy is nerve damage caused specifically by diabetes. Peripheral neuropathy can happen for many reasons — diabetes being one of them. In medical coding, diabetic peripheral neuropathy ICD 10 falls under E11.42.
9. How can I prevent diabetic neuropathy?
Keep blood sugar levels stable, eat a healthy diet, exercise regularly, and avoid smoking or heavy alcohol use. Regular checkups help doctors track progress using your ICD-10 diabetic neuropathy code and adjust your care plan as needed.
10. Is ICD-10 used worldwide?
The ICD-10 system is used worldwide, but the ICD-10-CM version (Clinical Modification) is specifically used in the United States for medical documentation and insurance billing.
Final Word
Whether it’s E11.40 or E11.42, every ICD-10 diabetic neuropathy code tells part of your story — one that’s shaped by awareness, care, and progress. The more you understand these codes, the better you can partner with your healthcare team to keep your nerves healthy and your future bright.