Discover how left bundle branch block (LBBB) affects your heart, its link to heart disease, symptoms, diagnosis, and the best treatment options.Heart Disease and Left Bundle Branch Block: Causes, Symptoms & Treatment
Understanding the Link Between Heart Disease and Left Bundle Branch Block
Imagine your heart as a house full of lights. Every time your heart beats, an electrical impulse flicks those lights on and off in perfect rhythm. But what if one side of the wiring slows down or gets blocked? That’s what happens in a left bundle branch block, often called LBBB. It’s not a heart attack, but it can signal that your heart’s electrical system needs attention.
A left bundle branch block happens when the electrical conduction in the heart slows or stops on the left side of your heart’s pumping system. Because of this, the left ventricle — the chamber that pushes blood out to your body — takes a little longer to contract. This delay may not sound serious, but over time it can affect how efficiently your heart pumps blood, especially if you already have heart disease or another underlying heart condition.
Now, here’s something important: not everyone with an LBBB feels symptoms. Some people find out by accident, like during a routine ECG (electrocardiogram). Others may experience signs such as tiredness, shortness of breath, or a fluttering heartbeat. These small clues can help catch bigger issues early — like coronary artery disease, heart failure, or other rhythm problems linked to bundle branch block.
You might be wondering, “Can a left bundle branch block cause heart disease?” In most cases, it’s the other way around — existing heart disease or damage from a heart attack can lead to a bundle branch block. However, ignoring it could make your heart work harder and increase the risk of complications later on.
The good news? With today’s technology, doctors can easily diagnose LBBB using an ECG test and, if needed, guide you toward the right treatment — whether it’s medication, a pacemaker, or lifestyle changes like exercise and heart-healthy eating.
So, while a left bundle branch block may sound alarming, it’s often a helpful warning light — a gentle nudge from your heart reminding you to listen closely and take care of it. After all, your heart’s rhythm is more than just a beat — it’s your life’s soundtrack.
How Left Bundle Branch Block Connects to Heart Disease
Your heart is more than just a muscle — it’s a tiny electrical power station. Every beat starts with a signal that travels through special “wires” inside your heart. These wires are called bundle branches, and they help both sides of your heart beat together, like two dancers moving in perfect sync. But when one side’s signal slows down — especially on the left — that’s when a left bundle branch block (LBBB) happens.
Now, you might ask, “How does this relate to heart disease?”
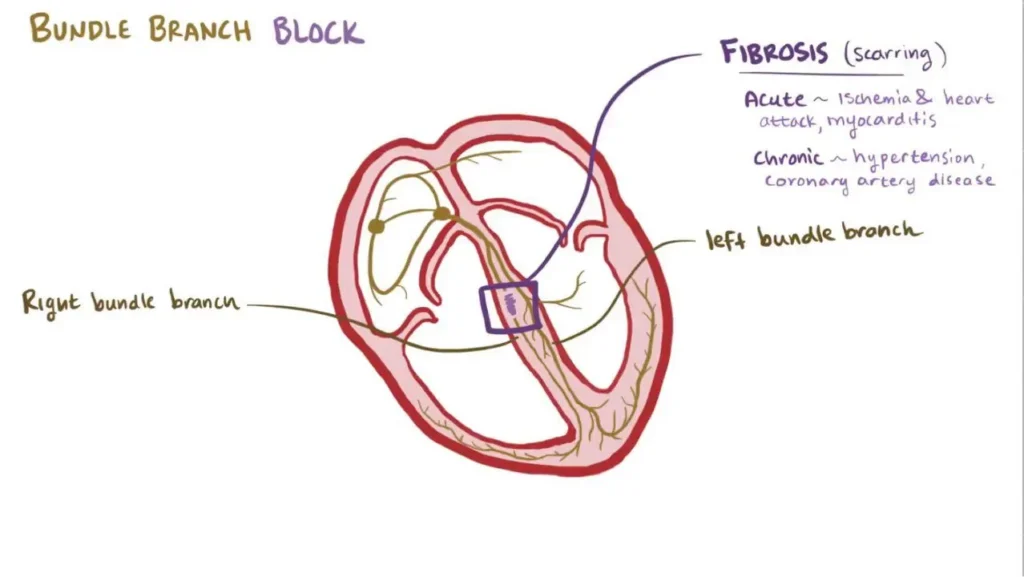
Well, the connection between LBBB and heart disease is pretty strong. In many cases, heart disease — especially coronary artery disease or heart failure — can damage the heart’s electrical pathway. When the tissue around the left bundle gets scarred or weakened, it disrupts those smooth electrical impulses that tell your heart when to pump.
Think of it like a traffic jam in your heart’s wiring system — the right side keeps moving, but the left side is delayed. This delay can cause your heart to beat out of rhythm or lose pumping strength. Over time, this makes the heart work harder, and that’s where heart failure or irregular heartbeat can start to develop.
In other words, left bundle branch block is often a symptom of underlying heart problems, not the cause. But here’s the tricky part — sometimes LBBB appears even when a person doesn’t have obvious heart disease. That’s why doctors pay close attention to it, using tests like an ECG (electrocardiogram), echocardiogram, or cardiac MRI to uncover what’s really going on inside your heart.
It’s also worth knowing that LBBB can make it harder for doctors to read certain ECG patterns, especially if they’re looking for a heart attack. That’s why getting the right diagnosis early is so important.
If you already have high blood pressure, diabetes, or a history of heart attack, your chances of developing a left bundle branch block increase. But don’t worry — the earlier it’s found, the better your doctor can guide you toward treatment and lifestyle steps to protect your heart.
Common Causes of Left Bundle Branch Block
Your heart works like a finely tuned orchestra — every section plays in rhythm, guided by tiny electrical signals. But when the “conductor” on the left side gets delayed, you have what’s known as a left bundle branch block (LBBB).
So, what causes this electrical hiccup in the heart’s rhythm? Let’s break it down simply.
One of the most common causes of left bundle branch block is heart disease — especially coronary artery disease. This happens when the arteries that feed your heart get narrowed or blocked, reducing the flow of oxygen-rich blood. Without enough oxygen, parts of the heart muscle can become weak or damaged, and that damage can affect the electrical conduction in the heart.
Another big reason is heart failure, where the heart struggles to pump blood efficiently. The strain from pumping harder can disrupt the heart’s internal “wiring system,” leading to a bundle branch block. In fact, many people with long-term heart failure also develop LBBB as their condition progresses.
Other possible causes include:
- High blood pressure (hypertension): Over time, it makes your heart muscle thicker and stiffer.
- Cardiomyopathy: A condition where your heart muscle becomes enlarged or weak.
- Previous heart attack: Scar tissue from a heart attack can block or slow electrical signals.
- Aging: As we grow older, the fibers that carry those impulses may wear out naturally.
- Heart valve disease: Especially aortic valve problems, which put pressure on the heart’s left side.
Sometimes, a left bundle branch block appears without any major heart disease — especially in older adults. Doctors call this “isolated LBBB.” While it might sound less serious, it still requires regular checkups to make sure it doesn’t hide a deeper issue.
You might wonder: Can lifestyle play a role? Absolutely. Poor diet, lack of exercise, smoking, and uncontrolled high blood pressure all increase your risk of both heart disease and LBBB.
Symptoms of Left Bundle Branch Block You Shouldn’t Ignore
Your heart is pretty good at sending signals when something isn’t right — you just have to listen.
A left bundle branch block (LBBB) doesn’t always shout its presence with obvious symptoms. Sometimes, it whispers. In fact, many people discover they have a left bundle branch block during a routine ECG (electrocardiogram) without ever feeling a thing.
Still, when symptoms do appear, they’re your heart’s way of saying, “Hey, I need some help!”
Here are some of the most common symptoms of left bundle branch block that deserve attention:
- Shortness of breath — Feeling out of breath even after mild activity could mean your heart isn’t pumping efficiently.
- Chest pain or pressure — Especially if it occurs during exercise or stress, it could signal heart disease or reduced blood flow.
- Dizziness or fainting spells — An irregular heartbeat caused by electrical conduction delay can affect blood flow to the brain.
- Irregular heartbeat or fluttering — You may feel your heart racing or skipping beats, which can indicate bundle branch block or other rhythm issues.
- Fatigue or weakness — When the heart works harder to pump, your energy levels drop faster.
Now, here’s the tricky part: LBBB symptoms often mimic those of other heart conditions, such as coronary artery disease or heart failure. That’s why many doctors emphasize early testing. A simple ECG can spot the delay in your heart’s signals even before major problems show up.
Some people ask, “When should I see a cardiologist?” The answer is simple — don’t wait for severe pain. If you notice even mild symptoms like unexplained tiredness, fluttering, or shortness of breath, it’s worth getting checked.
Ignoring the signs of a left bundle branch block may allow an underlying heart condition — such as high blood pressure, heart attack, or valve disease — to progress quietly. But catching it early gives you a huge advantage.
How Doctors Diagnose Left Bundle Branch Block
When it comes to your heart, every beat tells a story — and doctors have tools that can read that story line by line. Diagnosing a left bundle branch block (LBBB) might sound complicated, but it’s actually done using simple, painless tests that reveal how your heart’s electrical system is working.
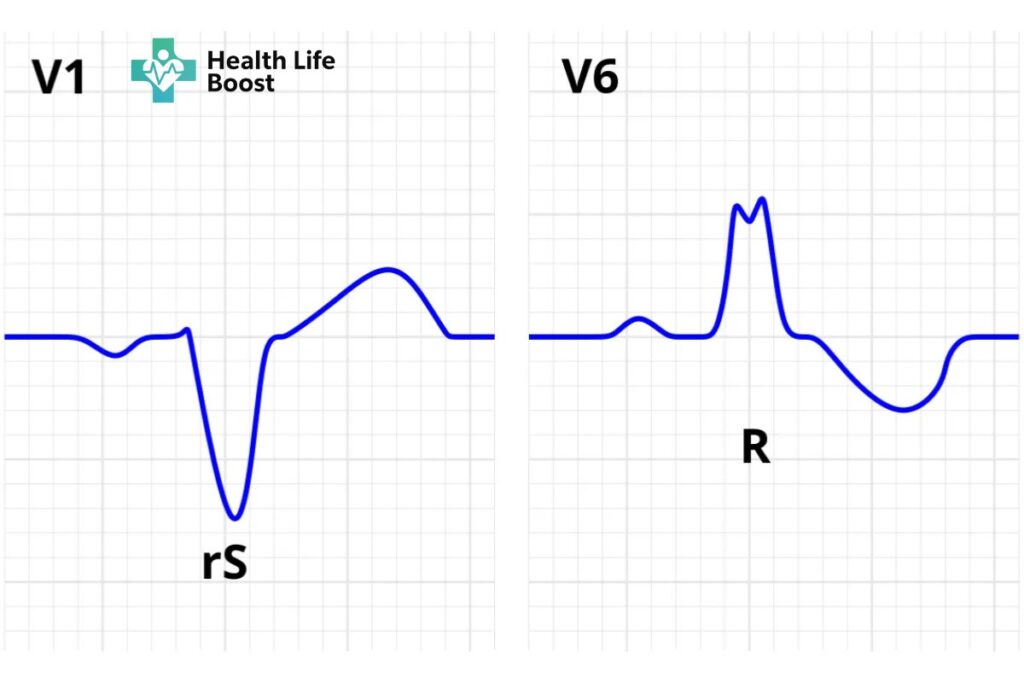
The most common test used to detect a left bundle branch block is an ECG (electrocardiogram). Think of it as a heart “snapshot.” Tiny sensors are placed on your chest, arms, and legs to measure the electrical impulses that control your heartbeat. On the ECG screen, these signals appear as lines and spikes. When a left bundle branch block is present, the pattern — called the QRS complex — looks wider or different than normal.
This unique pattern helps doctors identify if the electrical signal in your heart’s left bundle branch is delayed or blocked. It’s like seeing a small traffic jam in your heart’s electrical highway.
But an ECG isn’t the only way to confirm what’s happening. To understand the bigger picture, your doctor may also recommend:
- Echocardiogram: This ultrasound test shows how well your heart’s chambers and valves are working. It helps find underlying heart conditions like heart failure or cardiomyopathy that can cause LBBB.
- Cardiac MRI or CT scan: These imaging tests provide detailed pictures of your heart’s structure and detect scar tissue from a heart attack or coronary artery disease.
- Stress test: Helps evaluate how your heart performs under physical activity, especially if heart disease is suspected.
- Blood tests: Used to check for heart damage, infections, or other issues that could contribute to a bundle branch block.
Sometimes, left bundle branch block can make diagnosing a heart attack tricky because it changes the ECG’s usual pattern. That’s why doctors rely on multiple tests to confirm what’s going on.
If you’ve been told you have LBBB, don’t panic. Many people live full, healthy lives after diagnosis. The key is understanding the cause — whether it’s coronary artery disease, high blood pressure, or an underlying heart condition — and working closely with your healthcare provider to manage it.
Knowledge really is power here. The sooner your LBBB is diagnosed, the sooner you and your doctor can create a plan to keep your heart strong, steady, and beating beautifully.
Treatment Options for Left Bundle Branch Block
Hearing that you have a left bundle branch block might sound scary — but don’t worry. In most cases, it’s not a life sentence. It’s your heart’s way of saying, “Hey, I need a little help here.” The good news? Modern medicine has plenty of ways to help your heart get back on track.
First, it’s important to understand this: LBBB treatment depends on what’s causing it. Doctors focus on treating the underlying heart disease rather than the block itself.
Here are the most common treatment options for left bundle branch block you might hear about:
1. Treating the Root Cause
If your LBBB is caused by high blood pressure, coronary artery disease, or heart failure, managing those conditions is the top priority.
- Doctors may prescribe medications such as ACE inhibitors, beta-blockers, or diuretics to lower blood pressure and ease the heart’s workload.
- Lifestyle changes like eating a heart-healthy diet, staying active, and cutting down on salt and processed foods can also make a huge difference.
2. Pacemaker or Cardiac Resynchronization Therapy (CRT)
When LBBB affects how well the left and right sides of your heart beat together, doctors may recommend a pacemaker or a special device called cardiac resynchronization therapy (CRT).
- A pacemaker helps regulate your heart rhythm, ensuring each beat happens at just the right time.
- CRT goes a step further — it sends tiny electrical signals to both sides of your heart, helping them beat in sync again.
These devices can dramatically improve symptoms like fatigue, breathlessness, and dizziness — and, in some cases, even boost heart function.
3. Managing Heart Disease and Lifestyle
Since LBBB often occurs alongside heart disease, lifestyle adjustments are just as important as medications.
- Quit smoking (your heart will thank you).
- Limit alcohol and caffeine.
- Get regular checkups with your cardiologist to monitor your heart rhythm.
4. Regular Monitoring
Even if your left bundle branch block doesn’t cause major symptoms, regular ECGs and echocardiograms help doctors track your heart’s health and catch any changes early.
Remember, the goal isn’t just to “fix” the left bundle branch block — it’s to protect your entire heart. With the right care, many people live long, active, and happy lives after diagnosis.
Lifestyle Tips for Living with Left Bundle Branch Block (LBBB)
Getting diagnosed with a left bundle branch block (LBBB) might feel overwhelming at first, but here’s the truth — with the right habits and mindset, you can live a full, active, and healthy life.
Your lifestyle plays a huge role in how well your heart functions, especially when dealing with heart disease or electrical conduction problems like LBBB.
Let’s look at some simple, science-backed ways to support your heart health every day:
1. Eat a Heart-Healthy Diet
Your plate can be your medicine.
- Choose whole grains, leafy greens, fruits, lean proteins, and healthy fats like olive oil or avocado.
- Limit foods high in salt, sugar, and saturated fats — they can worsen high blood pressure and increase strain on your heart.
- The Mediterranean diet is a great option; it’s proven to lower the risk of coronary artery disease and other heart conditions often linked with LBBB.
2. Stay Physically Active
Exercise doesn’t just strengthen your muscles — it strengthens your heart too.
- Aim for at least 30 minutes of moderate activity most days, like walking, swimming, or cycling.
- If you have LBBB or heart failure, talk to your doctor before starting new workouts. They can suggest safe options that keep your heart in rhythm.
3. 15 Quit Smoking and Limit Alcohol
Smoking narrows your blood vessels and increases the risk of heart disease. If you smoke, this is your sign to quit.
- Even reducing alcohol can help lower blood pressure and improve overall heart function.
4. Manage Stress and Get Enough Sleep
Stress causes your heart rate and blood pressure to rise — not great news for someone with LBBB.
- Try deep breathing, meditation, or even just listening to relaxing music.
- Aim for 7–8 hours of quality sleep each night; your heart needs rest just like you do.
5. Keep Up with Regular Checkups
Don’t skip your doctor visits. Regular ECG and echocardiogram tests help track how your left bundle branch block is progressing.
- If you have a pacemaker or cardiac resynchronization device, your doctor will monitor it to make sure it’s working correctly.
6. Listen to Your Body
If you ever feel chest pain, shortness of breath, or sudden dizziness, don’t ignore it. These could be signs of a more serious heart problem like coronary artery disease or a heart attack. Always play it safe — call your doctor or emergency services.
When to See a Doctor for Left Bundle Branch Block
When it comes to your heart, timing matters — literally. Many people with a left bundle branch block (LBBB) don’t notice any symptoms at first, but that doesn’t mean it should be ignored. Even if you feel fine, it’s important to know when to reach out to your doctor. Your heart may be quietly asking for help before bigger problems appear.
Here are some signs it’s time to make that appointment — or even call for immediate medical attention:
1. New or Worsening Chest Pain
If you ever feel pressure, heaviness, or pain in your chest — especially during exercise or stress — seek medical help right away. These can be warning signs of coronary artery disease or a heart attack, both of which are closely linked with LBBB.
2. Shortness of Breath or Fatigue
Feeling winded after light activity or noticing unexplained tiredness could mean your heart isn’t pumping efficiently. This might be due to heart failure or poor electrical conduction caused by a left bundle branch block.
3. Dizziness, Lightheadedness, or Fainting
If your heart’s rhythm is irregular, your brain may not get enough oxygen. Don’t brush off dizzy spells or fainting — they’re your body’s way of waving a red flag.
4. Irregular Heartbeat or Palpitations
A racing or skipping heartbeat can feel strange — almost like your heart is “flipping” inside your chest. These sensations might signal a bundle branch block or another arrhythmia that needs medical evaluation.
5. Routine Monitoring
Even if you don’t have symptoms, regular ECG (electrocardiogram) tests are important once you’ve been diagnosed with LBBB.
Your doctor can track any changes and check for underlying heart disease such as high blood pressure, valve disorders, or cardiomyopathy.
Why Early Action Matters
Catching left bundle branch block early gives your doctor the best chance to treat or prevent complications. It can help uncover hidden heart conditions, prevent heart failure, and protect your heart rhythm before it becomes dangerous.
Remember, your body whispers before it screams — so listen to those whispers. Whether it’s mild chest discomfort, fatigue, or just something that “feels off,” it’s always better to get checked.
Complications and Risks of Left Bundle Branch Block
A left bundle branch block (LBBB) might sound harmless at first — after all, many people have it without major symptoms. But here’s the truth: while LBBB itself doesn’t always cause problems, it can be a sign that your heart’s electrical system or muscle is under stress. Understanding the possible complications can help you take early action and keep your heart safe.
Let’s look at what can happen if a left bundle branch block is left unmanaged or linked to other heart diseases.
1. Heart Failure
One of the most common risks of LBBB is heart failure — a condition where the heart can’t pump blood as well as it should. Because the left and right sides of the heart beat out of sync in LBBB, it can reduce the heart’s efficiency over time.
This can lead to symptoms like:
- Shortness of breath
- Swelling in the legs or feet
- Fatigue and weakness
If LBBB is combined with high blood pressure, coronary artery disease, or cardiomyopathy, the risk increases even more.
2. Irregular Heart Rhythms (Arrhythmias)
Left bundle branch block can disrupt your heart’s timing, leading to arrhythmias — irregular or skipped beats. Some arrhythmias are harmless, but others can cause dizziness, fainting, or even sudden cardiac arrest in severe cases.
3. Difficulty Diagnosing Heart Attacks
Here’s a surprising one — LBBB can make it harder for doctors to identify a heart attack on an ECG (electrocardiogram) because it changes the usual wave patterns. That’s why people with LBBB are often monitored more closely and may need additional tests like echocardiograms or cardiac MRIs to confirm what’s happening inside the heart.
4. Progressive Heart Disease
Sometimes, LBBB develops as a result of an existing condition — and over time, it can worsen if the root cause isn’t treated. It can also be an early warning sign of coronary artery disease, valve disorders, or degenerative changes in the heart’s electrical pathways.
5. Reduced Quality of Life
Even mild LBBB can affect your day-to-day energy and comfort. You might find yourself feeling more tired, lightheaded, or easily winded. These symptoms can take an emotional toll, especially if you’re used to being active. But the good news? With the right treatment plan, most people regain their strength and live full, happy lives.
Prevention and Long-Term Heart Health Tips
You can’t always control what happens inside your heart — but you can give it the best chance to thrive.
Whether you’ve already been diagnosed with a left bundle branch block (LBBB) or simply want to prevent heart disease, the secret to long-term heart health lies in consistency and care.
Here’s how to keep your heart beating strong and steady for years to come:
1. Eat Smart, Not Strict
A heart-healthy diet isn’t about perfection — it’s about balance.
- Choose fresh fruits, vegetables, whole grains, and lean proteins like fish or chicken.
- Limit processed foods, salt, and saturated fats — they can raise blood pressure and strain your heart.
- Add omega-3-rich foods (like salmon or walnuts) to reduce inflammation and support your heart rhythm.
Every bite can either hurt or heal your heart — make it count.
2. Keep Moving
Your heart loves movement!
- Try 30 minutes of light to moderate exercise most days of the week — walking, swimming, or yoga are great choices.
- If you have LBBB, talk to your doctor before starting new workouts. They can suggest a safe plan tailored to your heart’s needs.
Exercise helps regulate blood pressure, improve circulation, and strengthen your heart muscle — all essential for managing left bundle branch block and preventing heart failure.
3. Quit Smoking & Limit Alcohol
Smoking damages your arteries and makes it harder for your heart to work efficiently. If you smoke, quitting is the best gift you can give your body.
And when it comes to alcohol, moderation is key. Too much can weaken the heart and worsen arrhythmias — irregular rhythms often linked to bundle branch block.
4. Prioritize Sleep and Stress Relief
Stress and lack of sleep are silent enemies of heart health.
- Practice deep breathing, prayer, or meditation to calm your mind.
- Get at least 7–8 hours of quality sleep every night.
Your heart needs rest just as much as it needs rhythm.
5. Regular Heart Checkups
Even if you feel fine, regular ECG (electrocardiogram) and echocardiogram tests help your doctor monitor changes in your heart’s rhythm and structure.
- Schedule checkups at least once or twice a year.
- If you already have LBBB, your doctor may adjust treatments or monitor your pacemaker or cardiac resynchronization therapy (CRT) device.
6. Know Your Numbers
Stay aware of your:
- Blood pressure
- Cholesterol levels
- Blood sugar levels
Keeping these in healthy ranges helps prevent coronary artery disease, heart attacks, and further conduction problems in your heart.
Final Thoughts
A left bundle branch block doesn’t have to control your life — it’s simply your heart asking for attention. By choosing healthy habits, following your doctor’s advice, and staying proactive, you can manage LBBB and reduce your risk of heart disease.